September 2025 Newsletter.
Welcome to our newsletter, with all our updates and some helpful resources for you. In this edition we talk about Greater Trochanteric Pain Syndrome (GTPS)
Remember, we are here to help you and you can contact us anytime.
Welcome to our
september newsletter
Hello Folks, welcome to our September newsletter,
As we say goodbye to a lovely hot summer, many of us will have enjoyed the chance to get outside — long walks, gardening, tennis, golf, or simply being more active in the sunshine. I know that I have enjoyed the opportunity for longer walks, morning yoga sessions in the garden and frequent swims down at Ringstead Bay. All this activity is fantastic for health and wellbeing, but it can also sometimes highlight those niggly aches and pains that creep up on us.
A particular highlight for our family this year was a trip to the Peak District where we enjoyed some lovely walks around Hathersage and Hope valley in Castleton.
The weather was stunning and allowed for some breathtaking views across the vales, it certainly blew away the cobwebs and has set us up for the months ahead.
I was particularly pleased as a personal goal of mine for this summer was to complete a walk like this having had my hip replaced in December, I walked with no pain, cleared all the styles with ease, kept up with the kids and enjoyed every minute! Hope you enjoy this months content have a happy healthy September,
All the best Samantha & Boris
As always we have our ‘community’ piece this month featuring Kate Mason and Julia Aston friends and patients of Ocean therapy who have recently completed some amazing open water challenges which we would like to share with you. They both completed a 20km Lake swim in Lake Serra, Poncon in the southern French Alps on July 5th this year.
Then Kate went on to swim the Gibraltar Straits from Tarifa Spain to the Moroccan Coast in Africa. Kate swam with Patrick Cray of Weyport Masters and completed the gruelling distance of 9 miles in 4 hours 32 mins. Kate went on to tell me that this crossing is only achievable when there is a westerly wind. She also commented on how skilled the skipper was crossing this notoriously busy shipping channel, what with challenging currents to navigate along with huge container ships. However Kate said it was worth the couple of days wait in Tarifa to fix the ideal conditions, and enjoyed her Gibralter Straits challenge…….Just amazing achievements ….what will it be next for these talented mermaids??
Greater Trochanteric Pain Syndrome
One condition we see quite regularly in the clinic is Greater Trochanteric Pain Syndrome (GTPS) — a common cause of pain on the outside of the hip. We thought that we would highlight this condition this month as we have had a few cases of it through the last month or so and thought the following information and advice may be of help to you or someone else that you may know.
WHAT is GTPS?
Hip pain is a common orthopaedic problem. Greater trochanteric pain syndrome (GTPS), previously known as trochanteric bursitis, affects 1.8 per 1000 patients annually[1].
GTPS is a clinical diagnosis of lateral hip pain and includes trochanteric bursitis associated with a tendinopathy, gluteusmedius (GMed)/ minimus (GMin) tendinopathy; tears of the gluteus medius or minimus tendons.
Patients complain of pain over the lateral aspect of the thigh that is exacerbated with prolonged sitting, climbing stairs, high impact physical activity, or lying over the affected area.
The main bursae that are associated with GPTS are the gluteus minimus, gluteus medius, and the gluteus maximus.
Previously, trochanteric bursitis was seen as the main pain source, but recent research indicates that the fluid within the bursa rather exists due to the gluteal tendinopathy and not because of primary inflammation in the bursa The most recent research indicates GMed and GMin tendinopathy as the most frequent cause of GTPS and managing the underlying tendinopathy should take priority.
Why does GTPS affect women so often?
GTPS is often linked to irritation of the tendons and soft tissues around the hip. While anyone can get it, we see a higher number of women, particularly as they go through the peri-menopause and menopause.
Hormonal changes at this stage of life can affect tendon health and muscle strength, making the hip region more vulnerable. Combine this with a summer of extra walking, exercise, and outdoor activities — and it’s no surprise that more people notice hip pain around now.
Typical Symptoms
· Pain or tenderness on the outside of the hip
· Discomfort lying on the affected side (especially at night)
· Pain climbing stairs or walking uphill
· Aching after long walks or standing for long periods
The Good News
With the right approach, GTPS responds very well to treatment. Key elements include:
Learning how to avoid positions that aggravate the tendon (like crossing your legs or lying directly on the sore side)
Simple strengthening exercises to improve hip stability
Advice on pacing activity so you stay active but don’t overload the hip
By addressing the root causes, most people can return to the activities they enjoy — whether that’s autumn walks, fitness classes, or just keeping up with day-to-day life.
Our Role in Your Recovery
At the clinic we specialise in helping people manage GTPS. We’ll assess your movement, identify contributing factors, and build a tailored plan to:
Reduce your pain
Restore strength
Keep you active long-term
Looking Ahead to Autumn
As the evenings draw in and our activity routines change, it’s the perfect time to look after your hips, joints, and general wellbeing. If you’ve been experiencing hip pain, or if those summer activities have left you with lingering soreness, don’t ignore it — come and see us.
We can help you stay mobile, comfortable, and ready to enjoy the months ahead. 🍂
You can also help yourself by being mindful of your diet, avoiding ultra processed food, and sugar will help to avoid unnecessary inflammation in the body , remember to stay hydrated too, consider supplements like fish oils and Omega’s which will help lubricate joints and keep them healthy.
A Quick Look at the Anatomy Behind GTPS
On the outside of your hip there’s a bony bump called the greater trochanter — you can often feel it if you press the side of your hip. Attached to this area are some important muscles and tendons, mainly the gluteus medius and gluteus minimus, which help keep your pelvis stable when you walk, climb stairs, or stand on one leg.
Sometimes, these tendons can become irritated or overloaded, leading to pain and tenderness in this area. There’s also a small fluid-filled cushion (called a bursa) that sits between the tendons and the bone, which can become sore if the tendons are aggravated.
The result? Pain on the outside of the hip, especially when lying on it, climbing stairs, or after long periods of walking or standing.
The good news: With the right exercises and habits, GTPS usually improves very well without injections or surgery.
Do’s & Don’ts
✅ Do:
Sleep with a pillow between your knees if lying on your side
Sit in a chair with your hips slightly higher than your knees
Walk regularly, but keep the distance manageable
Do your exercises daily (phased programme below)
❌ Don’t:
Sit cross-legged
Stand with your hip “popped out” to one side
Lie on the painful hip without support
Suddenly increase activity (long walks, steep hills, or stairs in one go)
Your Exercise Programme
Follow the programme in phases. Stay in each phase until you can do the exercises comfortably before moving to the next.
Phase 1: Pain Relief & Protection (Weeks 0–2)
Isometric Glute Press (press thigh gently into pillow/wall) – 5×20 sec
Bridge (glute squeeze, lift hips slightly) – 2×10 reps
Clam (knees bent, gently lift top knee) – 2×10 reps
Leg lifts ( lying face down activate gluteals, lift , hold for 3 seconds release , deactivate )- x2 x10 reps
Be mindful of activating your glutes throughout daily activities , walking etc
Hamstring stretches ( as demonstrated)
Global postural awareness
Phase 2: Muscle Activation & Gentle Strength (Weeks 2–6)
Side-lying leg lifts (short range, controlled) – 3×10 reps
Clam with resistance band – 3×12 reps
Bridge with band around knees – 3×10 reps
Step-ups (low step) – 3×10 reps
Balance on one leg (hold support if needed) – 30 sec × 3
Phase 3: Functional Strength & Stability (Weeks 6–12)
· Side-steps with resistance band – 3×12 steps each way
· Single-leg bridges – 3×10 reps each side
· Hip hikes (stand on step, lift/drop opposite hip) – 3×10
· Monster walks with band – 3×10 steps forward/backward
· Progress step-ups (higher step or add weight) – 3×10 reps
Phase 4: Return to Activity (12+ weeks)
Brisk walking, cycling, swimming, or pool walking
Continue hip strengthening 2×/week long-term
Build up slowly – avoid big sudden increases in activity
Lifestyle Tips
Walk daily, but spread activity across the week
Keep your hips and core strong with regular exercise
Maintain good posture when sitting and standing
Manage bodyweight if advised by your healthcare team
Keep a ‘pain ‘diary and report to your team regularly
Quick Checklist
☑ I avoid sitting cross-legged
☑ I use a pillow between my knees at night
☑ I do my phase exercises every day
☑ I walk regularly without overdoing it
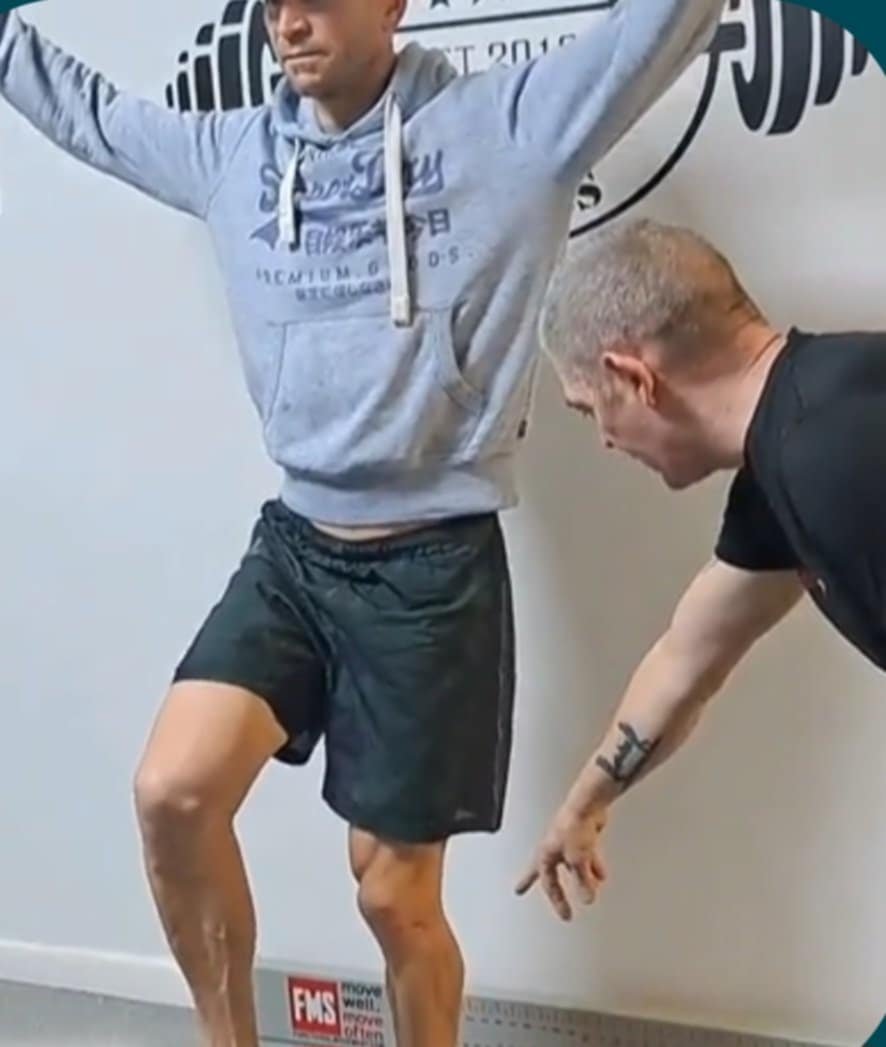
Unlocking the Power of Functional Movement Assessments: Preventing and Recovering from Injuries
Often most people think of assessments in a clinical setting, they picture checklists of symptoms, range-of-motion measurements, or strength tests for specific muscles. While these traditional assessments are important, they don’t always reveal the bigger picture—how your body actually moves as a whole. That’s where functional movement assessments (FMAs) come in.
Unlike standard clinical tests that often isolate a joint or muscle, functional movement assessments evaluate how the entire body works together during real-life movements. Think of it as looking at the way your body moves in action, rather than just how individual parts perform in isolation.
Why Functional Movement Assessments Matter
Movement is rarely about just one muscle or joint. Whether you’re lifting groceries, running, or sitting at your desk, multiple systems—muscular, skeletal, and neural—are working in sync. If there’s a breakdown anywhere along the chain, it can create compensations that may not cause pain immediately but could set you up for future injury.
A functional movement assessment can identify:
• Muscle imbalances (overactive vs. underactive muscles)
• Movement compensations (the body “cheating” to complete a task)
• Mobility or stability restrictions that affect performance
• Asymmetries between the left and right sides of the body
By spotting these issues early, we can address them before they develop into injuries—making FMAs a valuable tool not only for rehabilitation but also for prevention.
From Assessment to Corrective Strategy
The beauty of a functional movement assessment is that it doesn’t stop at identifying problems; it gives us a roadmap for correction.
Here’s how it works in practice:
• Assessment – You complete a series of movement patterns (like squats, lunges, or reaches) while we observe compensations and limitations.
• Analysis – We pinpoint which muscles are tight, which are weak, and how your body is compensating.
• Plan – Based on this, we create a tailored corrective exercise program. This might include mobility drills to improve range of motion, activation exercises to “wake up” underactive muscles, and stability or strength work to reinforce proper movement patterns.
• Progression – As imbalances correct and movement efficiency improves, we can gradually progress your program back to performance-focused training.
Prevention Meets Rehabilitation
Functional movement assessments aren’t just for those recovering from injuries. They’re equally powerful for healthy individuals looking to stay injury-free. By regularly screening movement, we can catch red flags early and adjust training programs to keep the body resilient.
For someone recovering from an injury, FMAs provide a bridge between rehab and performance. Rather than only focusing on pain-free range of motion, we ensure that movement patterns are restored so the same injury doesn’t reoccur.
The Takeaway
Functional movement assessments go beyond what traditional clinical evaluations can show. They give us a clearer picture of how the body truly functions, helping us prevent injuries before they happen and accelerate recovery when they do.
By identifying imbalances and designing a corrective exercise rehab plan, we don’t just treat symptoms—we address root causes, restore balance, and set the stage for long-term health and performance.
Boris is a Corrective Exercise Specialist with over 25 years of experience in this field. To book an assessment with Boris, call the office at OceanTherapy on 01305 831726.