February 2026 Newsletter.
Welcome to our newsletter, with all our updates and some helpful resources for you. In this edition we talk about the Trendelenburg sign.
Remember, we are here to help you and you can contact us anytime.
Welcome to our
february newsletter
Hello Ocean therapy friends!!
Welcome to our February edition.
As I write this, we’re nearing the end of a very bleak January — grey skies, relentless rain, flooding and mud. For many of us, the slow shift into February feels like a welcome one.
I’ve taken the opportunity to hibernate where possible, embracing the cold, wet evenings with a good book beside the log burner, plenty of tea (it’s been a dry January for me!) and the last slice of Christmas cake.
Personally, it’s been a month of reflection and gratitude as I’ve looked back on the year and what I achieved. As many of you know, I entered 2025 with a replacement hip. Later in the year, I launched a virtual Hip Coaching Programme for those who don’t live locally but would benefit from personalised support and guidance.
It’s still in its pilot phase, so if you know anyone struggling with a hip diagnosis or recovery, please do send them my way.
We are supporting a dear friend and patient of Ocean therapy this month whilst she raises funds for cancer research UK. Claire has undertaken the task of completing 100 squats a day in February!!!! (No easy task). We all know someone who has been affected by cancer so if you can please donate using the following link: All monies are very gratefully received thank you x ( Remember Claire, we have promised you a complimentary treatment when you have finished to treat those tired limbs!!!!)
Donate here: https://fundraise.cancerresearchuk.org/page/claires-giving-page-14095220
What’s in this newsletter? Leading on from our gluteal strength advice seen in previous newsletters and for our on going Hip replacement information this month, we discuss the Trendelenburg sign and we accompany this with some interesting patient information resources on health and wellbeing with some top tips on how to look after yourself as we progress through the winter months.
Why February Is the Perfect Time to Rethink How You Treat Pain and Injury?
February is often the point where motivation starts to dip. New Year training plans are underway, but so are the familiar aches, pains, and recurring injuries. For many people, this is when they realise something important: Exercise alone isn’t fixing the problem. As a corrective exercise specialist and sports therapist, one of the most common things I see is people working hard in the gym or following rehab exercises—but still feeling stuck in pain. That’s usually because the root cause hasn’t been identified.
This is where functional movement assessments come in.
What Is a Functional Movement Assessment?
A functional movement assessment looks at how your body moves as a whole, not just where it hurts. Instead of isolating one joint or muscle, we assess:
• How you walk, squat, hinge, lunge, push, and rotate
• How joints interact with each other
• Where your body compensates to create movement
• Which areas lack mobility and which lack stability
Pain is often the end result of a movement problem—not the source of it.
How This Differs From Traditional Therapy Assessments
Traditional therapy or injury assessments often focus on:
• The site of pain
• Local strength or flexibility
• Passive testing
While this can be useful, it doesn’t always show what happens when your body is upright, loaded, and moving—which is how pain and injury usually develop. A functional movement assessment is different because it:
✔️ Assesses movement, not just muscles
✔️ Looks at how the whole body works together
✔️ Identifies compensation patterns
✔️ Reflects real-life movement demands
Why “Ordinary Exercises” Can Make Things Worse
If you train or rehab without addressing movement faults, your body will simply find another way to complete the task. Over time, this reinforces poor patterns, overloads joints, and keeps you stuck in a cycle of pain.
From Assessment to Action: Corrective Exercise Plans
Once movement imbalances are identified, we can build a corrective exercise plan that restores proper function—starting from the ground up.
Foot and Ankle: The Foundation
Knee Position: Control, Not Just Strength
Hip Position: The Key Link
By improving movement at the foot and ankle, correcting knee alignment, and restoring hip function, we can often reduce stress on the lower back and joints—and in many cases, treat back pain without directly working on the back itself.
How Boris Can Help (And You Don’t Have to Be a Sports Person)
One of the biggest misconceptions about sports therapy and movement assessments is that they’re only for athletes.
That simply isn’t true.
You don’t have to play sport, go to the gym, or consider yourself “active” for Boris to help you. Boris works with:
• People who sit for long hours at work
• Individuals struggling with everyday aches and pains
• Those recovering from injury or surgery
• People who just want to move better and feel more comfortable day to day Through a detailed functional movement assessment, Boris can:
• Identify the real source of your pain
• Highlight movement restrictions caused by lifestyle, work, or previous injuries
• Explain why pain keeps returning—even if you’re “not doing much”
From there, Boris creates a personalised corrective exercise programme that fits your life, not a one-size-fits-all plan.
The goal isn’t to turn you into an athlete—it’s to help you:
✔️ Move more freely
✔️ Reduce pain
✔️ Improve confidence in everyday movement
✔️ Prevent future problems
Treating the Cause, Not the Symptoms
Whether you’re an athlete or not, your body follows the same movement principles. When those principles are compromised, pain shows up. Functional movement assessments allow us to correct those issues at the source—so you’re not just coping with pain, but actually resolving it.
Final Thoughts for February If pain keeps returning, it’s rarely because you’re not doing enough. More often, it’s because your body needs: Better movement, not more effort. And that applies to everyone. With the right assessment and a targeted corrective exercise plan, lasting change is possible—and Boris is here to help, no matter your activity level.
To book a functional movement assessment and rehab/ prehab plan, Book in with Boris at Ocean Therapy On 01305 831726
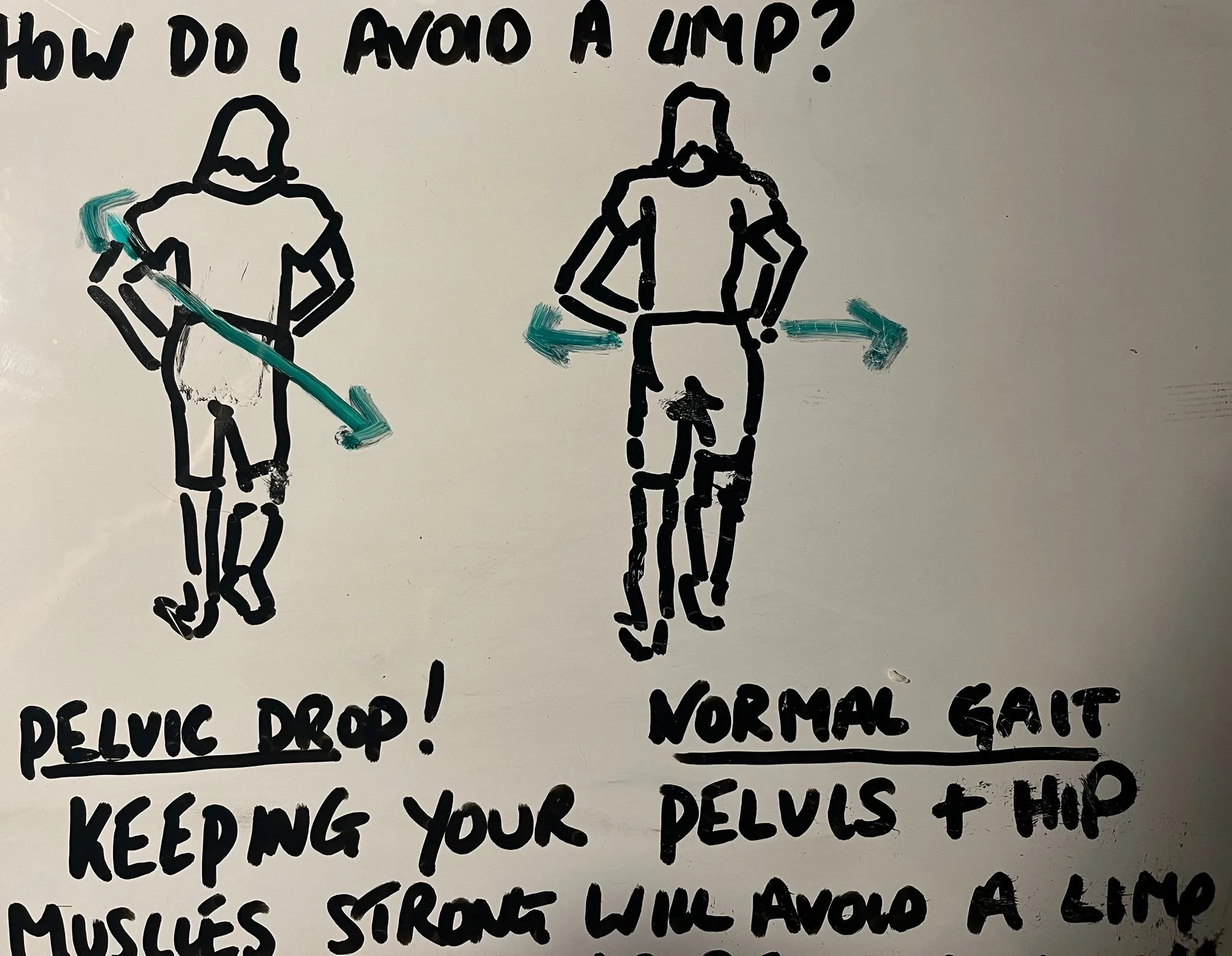
Understanding the Trendelenburg Sign: Your Guide to Preventing Hip-Related Limping
Walking is something most of us take for granted—until something goes wrong.
If you've noticed a hip drop or side-to-side sway when you walk, or if someone has mentioned you have a "waddle" in your gait, you might be experiencing what medical professionals call a Trendelenburg sign.
The good news? With the right knowledge and exercises, you can correct this pattern and walk with confidence again.
What Is the Trendelenburg Sign?
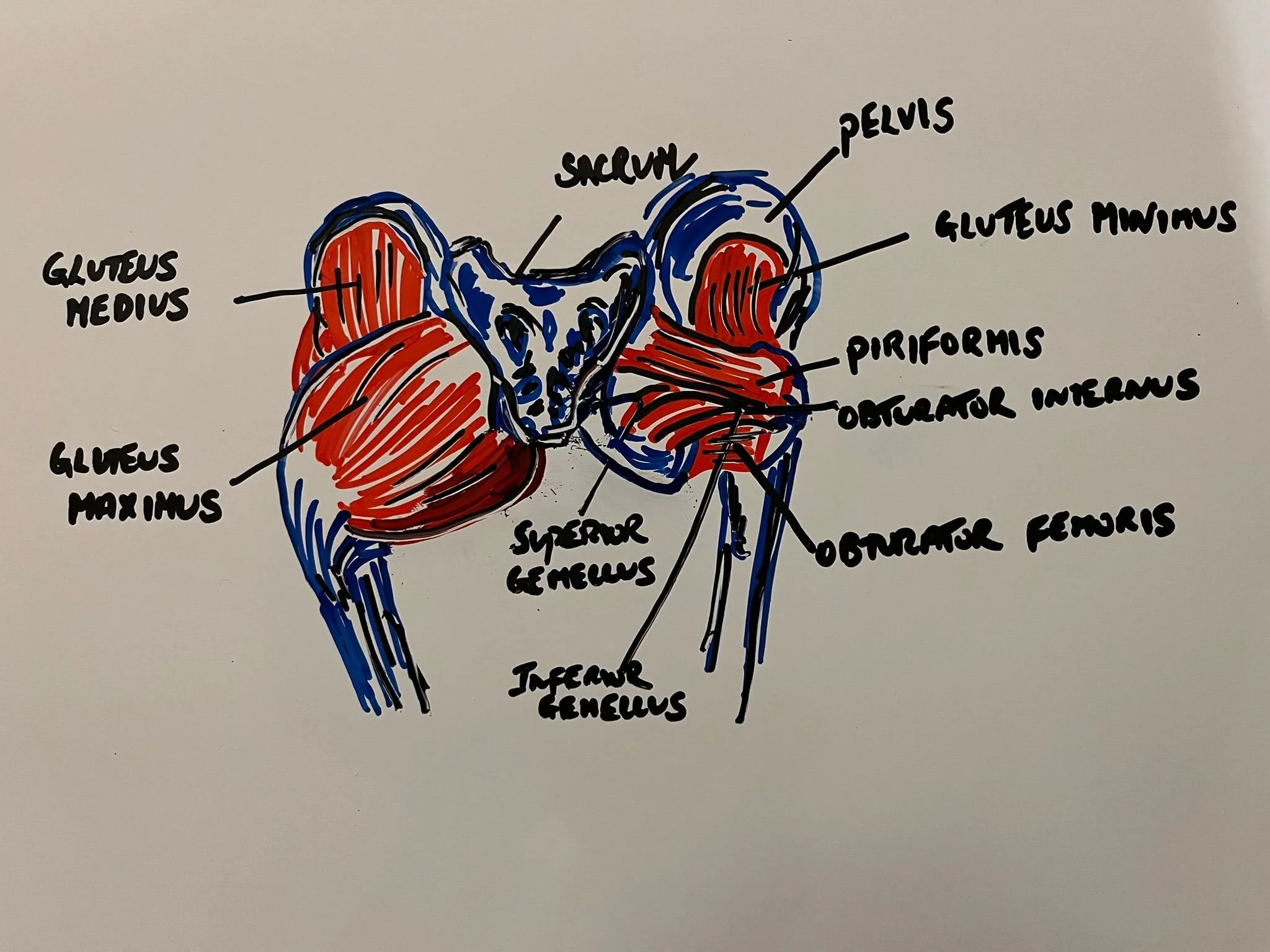
Named after German surgeon Friedrich Trendelenburg who first described it in 1897, the Trendelenburg sign is a clinical finding that indicates weakness in your hip abductor muscles—primarily the gluteus medius and gluteus minimus.
These muscles are the unsung heroes of walking, responsible for keeping your pelvis level when you stand on one leg.
During normal walking, when you lift one foot off the ground, the hip muscles on your standing leg work hard to keep your pelvis stable.
When these muscles are weak or not functioning properly, your pelvis drops toward the side of the lifted leg, creating the characteristic Trendelenburg gait pattern.
(StatPearls - NCBI)
Two Types of Trendelenburg Gait
Uncompensated Trendelenburg:
The pelvis visibly drops on the side of the swinging leg during walking
Compensated Trendelenburg:
The body leans toward the standing leg to bring the center of mass over the supporting foot—a compensation strategy to make walking easier
Both patterns indicate that your hip abductors aren't functioning optimally, and over time, this can lead to pain in your hips, lower back, knees, or SI joints.
(The Prehab Guys)
What Causes a Trendelenburg Sign?
A positive Trendelenburg sign can result from various conditions:
Structural Issues:
Hip dislocation or subluxation
Hip osteoarthritis
Femoral neck or greater trochanter fractures
Coxa vara (abnormal hip angle)
Legg-Calvé-Perthes disease
Neuromuscular Causes:
Superior gluteal nerve damage (often from surgery or injury)
Polio
Muscular dystrophy
Hemiplegic cerebral palsy
Other Contributors:
Lower back pain
Post-hip replacement surgery recovery
Short leg syndrome
Painful hip conditions causing muscle inhibition
(StatPearls - NCBI)
Why Should You Care?
Beyond the aesthetic concern of an abnormal gait, a Trendelenburg pattern can have serious consequences:
Increased injury risk:
Athletes with weaker hip abduction strength are more likely to sustain injuries in sports like soccer, ice hockey, and running
Chronic pain:
The compensatory movement patterns can lead to pain throughout the kinetic chain—from your ankles to your lower back
Reduced performance:
Hip weakness limits your athletic potential and daily function
Progressive deterioration:
Without intervention, the gait pattern can worsen over time
The key to correcting a Trendelenburg gait lies in a three-phase approach: activation, strengthening, and movement retraining.
Here's your roadmap to better hip function:
Phase 1: Activation Exercises
Before you can strengthen a muscle, you need to "wake it up."
The gluteus medius often has poor representation in the brain's motor cortex, making it difficult to recruit properly.
Hip Dip and Raise Exercise:
Stand with your affected leg on a step or platform
Allow your pelvis to drop on the elevated leg side
Use your standing leg's hip muscles to raise the pelvis back to neutral
Focus on quality over quantity—this is about motor control, not just strength
Use a mirror initially to ensure proper form
Perform multiple repetitions to build that brain-muscle connection
This exercise activates the gluteus medius at 57-59%
of maximal voluntary contraction—excellent for retraining!
**See video for demonstration**
(The Prehab Guys)
Phase 2: Strengthening Exercises
Once activated, these muscles need to build strength and endurance.
Research shows these exercises provide the highest muscle activation:
1. Side Plank with Hip Abduction (89-103% MVIC)
Lie on your side with elbow under shoulder
Lift hips off the ground into a side plank
Raise your top leg toward the ceiling while maintaining the plank
This is the gold standard for gluteus medius activation!
2. Clamshells (62-77% MVIC)
Lie on your side with knees bent and feet together
Loop a resistance band around both knees
Open the top knee while keeping feet together
Control the movement back down
3. Side-Lying Hip Abduction (56% MVIC)
Lie on your side with legs straight
Raise your top leg toward the ceiling
Keep your hips stacked and avoid rotating backward
Lower with control and repeat
Phase 3: Movement Retraining
Strength alone won't fix the problem—you need to train your muscles to fire at the right time during functional movements.
Captain Morgan Exercise:
Stand near a wall on one leg
Place the opposite foot against the wall
Let your pelvis sink on the side away from the wall
Push back into the wall by engaging your hip muscles
This teaches dynamic pelvic control
Standing Fire Hydrants:
Stand on one leg (use support if needed)
Lift the other leg out to the side
Keep your pelvis level throughout—this is crucial!
Hold positions statically to strengthen the motor pathway
Single-Leg Squats:
Stand on one leg
Perform a controlled squat while maintaining knee alignment
Focus on keeping your pelvis level and knee tracking over your toes
Use visual feedback (mirror) or verbal cues initially
Additional Prevention Strategies
Beyond exercises, consider these approaches:
Pain Management:
Over-the-counter NSAIDs for inflammation
In severe cases, cortisone injections may be recommended by your physician
Address any underlying hip pain that might be causing muscle inhibition
Biomechanical Corrections:
Shoe lifts for leg length discrepancies
Proper footwear with good support
Gait analysis and functional testing by a physical therapist
Professional Support:
Physical therapy for guided rehabilitation
Biofeedback using electromyography to understand muscle activation
Osteopathic manipulative treatment for associated dysfunctions
The Bottom Line:
The Trendelenburg sign is more than just an awkward walk—it's your body signaling that your hip stabilizers need attention.
The good news is that with consistent, targeted exercises focusing on activation, strengthening, and movement retraining, most people can significantly improve or completely correct their gait pattern.
Remember: motor control is just as important as strength.
You need to retrain your brain-muscle connection through repetition and focused practice. All the hip strength in the world won't help if the muscle doesn't activate at the right time during walking!
If you're experiencing hip pain, persistent gait abnormalities, or have had recent hip surgery, consult with a physical therapist or healthcare provider. They can assess your specific situation and create a personalized rehabilitation program to get you walking smoothly again.
Start today with the hip dip and raise exercise, and take the first step toward a stronger, more stable gait!
Hip Dip and Raise Exercise:
Remember we are working the leg that is weight bearing / that is on the step ) start with 5 reps progressing up to 10/15 - 2-3 sets. Quality over quantity and remember your posture !!
Don’t forget! we are selling our gift vouchers in the reception, call in to reception on: 01305 831726 for more information.
As always if you require any further advice or have any questions relating to this or any other Injury’s or conditions, we are always available for a no obligation chat just call our receptionists on : 01305 831726 to arrange. Enjoy the next mointh or so…Spring is on it’s way! Stay safe,
Warmest wishes, Samantha & Boris
🌅 Stay Connected 🌅
Follow us on social media for monthly movement tips, clinic updates, and inspiration from our amazing Weymouth community.
📍 OceanTherapy Soft Tissue Injury Clinic, Weymouth, Dorset 📞 01305 831726

Disclaimer: This content is designed for information and education purposes only and is not intended as medical advice. Always consult with a qualified healthcare provider before beginning any exercise program, especially if you have existing medical conditions or concerns.